Evidence-based research has shown there’s a distinct gap in patient care, between the demand for treatment and those who receive it. For many years, the hurdle was getting telehealth to be seen more as a main form of accessing care, rather than an option behind primary care and physical health. Mental health and addiction specialists have fought for the distinct needs of their patients, and ways to improve the access and utilization of virtual healthcare services, with the hopes of also aiming to stop this gap from widening further.
The coronavirus pandemic has severely limited and isolated people who are needing or already receiving care for mental health or addiction, such as in-person care visits, in-person meetings at a rehab facility, support groups, and other important resources. Thus, new challenges and struggles have made it difficult to search and find alternative sources of care. As a result, this departure from routine, the fear of the unknown, and social isolation have exacerbated people’s stress, anxiety, depression, if not already pre-existing.
Now, in 2021, as statistics show, teletherapy services among healthcare providers seem to have become a promising strategy to improve the access to high-quality mental health and substance abuse treatment. The healthcare industry has continued to make progress toward providing people with the help they need and defining what that quality care looks like. Standards for how healthcare providers measure the quality of patient outcomes can be supported by various telehealth/teletherapy trends shown during the emergence of the COVID-19 pandemic.
To better understand this utilization of telehealth services, Northbound Treatment Services surveyed 600 medical professionals authorized to offer teletherapy services. Specifically, our team analyzed:
- Their willingness to prescribe medication virtually
- Whether they believe teletherapy is an effective means for counseling
- How their mental health has fared throughout the coronavirus pandemic
Keep reading to see what we found.
Key Findings
- There’s a significant change in respondents’ willingness (43%) to prescribe or recommend medication via virtual therapy.
- Less than 17% believe teletherapy treatment is “somewhat more effective” vs. in-person counseling.
- Technical difficulties (50%), home distractions (48%), and a client’s ability to be in the moment (47%) are among the top challenges medical professionals face when treating clients virtually.
- 44% of medical professionals have experienced an increase in no-show appointments since offering teletherapy.
- One-fourth (25%) rate their mental health as “somewhat worse” amid the coronavirus pandemic.
Medical Professionals Experience Reluctancy When Prescribing Medication Via Virtual Therapy
Since 2008, The Ryan Haight Online Pharmacy Consumer Protection Act (known as the Haight Act) has prevented healthcare providers from prescribing pain medication (opioids) via telehealth. This act also restricts access to prescribing medications that are used to treat chronic conditions that can be examined by a licensed physician through virtual visits and monitoring.
Our participants stated that they tend to be more reluctant to prescribe medication when treating their patients virtually than in-person due to the barriers they have faced. Healthcare providers are allowed to safely prescribe certain medications and monitor a person’s vitals utilizing telehealth technologies only if they first conduct an in-person exam with the patient, or if the patient is being treated at a facility that is registered by the Drug Enforcement Administration (DEA).
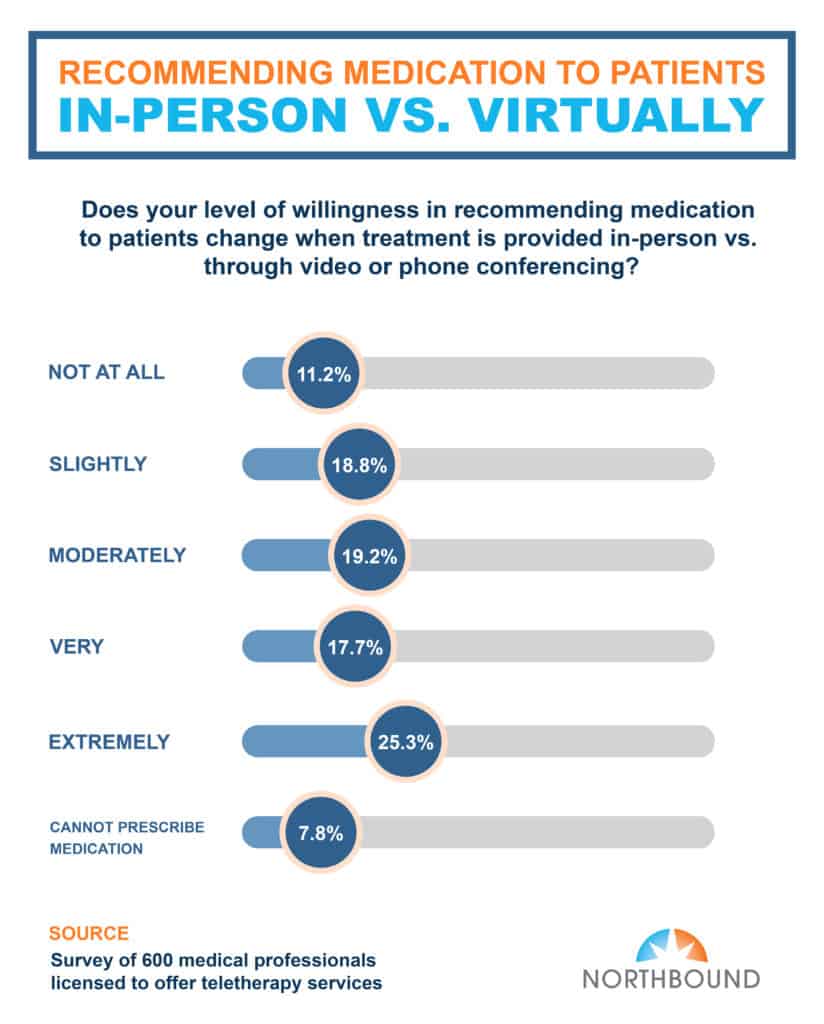
Our survey findings indicate that there was a significant change in respondents’ willingness (43%) to prescribe or recommend medication via virtual therapy. Eighty-one percent indicated on a scale from slightly, moderately, very, extremely that their decision to recommend or prescribe medication when using telehealth services is impacted.
Quality of Treatment Provided During Virtual Counseling vs. In-Person Therapy Sessions Remains Up for Debate
The measurement of treatment quality stands arguable when it comes to virtual versus in-person patient visits. Counseling can of course range across a variety of mental health conditions, such as mood and personality disorders.
What is the main difference between online therapy and in-person therapy? The answer is the type of communication that is used. In-person sessions happen face-to-face with the healthcare provider, where body language and nonverbal cues are picked up on. On the other hand, virtual counseling sessions are done via video conferencing, phone, or text, depending on the patient’s capabilities and preference.
However, whether someone with a mental disorder prefers virtual or in-person therapy remains up for debate. Forty-four percent of medical professionals who partook in our survey said they have experienced an increase in no-show appointments, upon offering virtual therapy treatment.
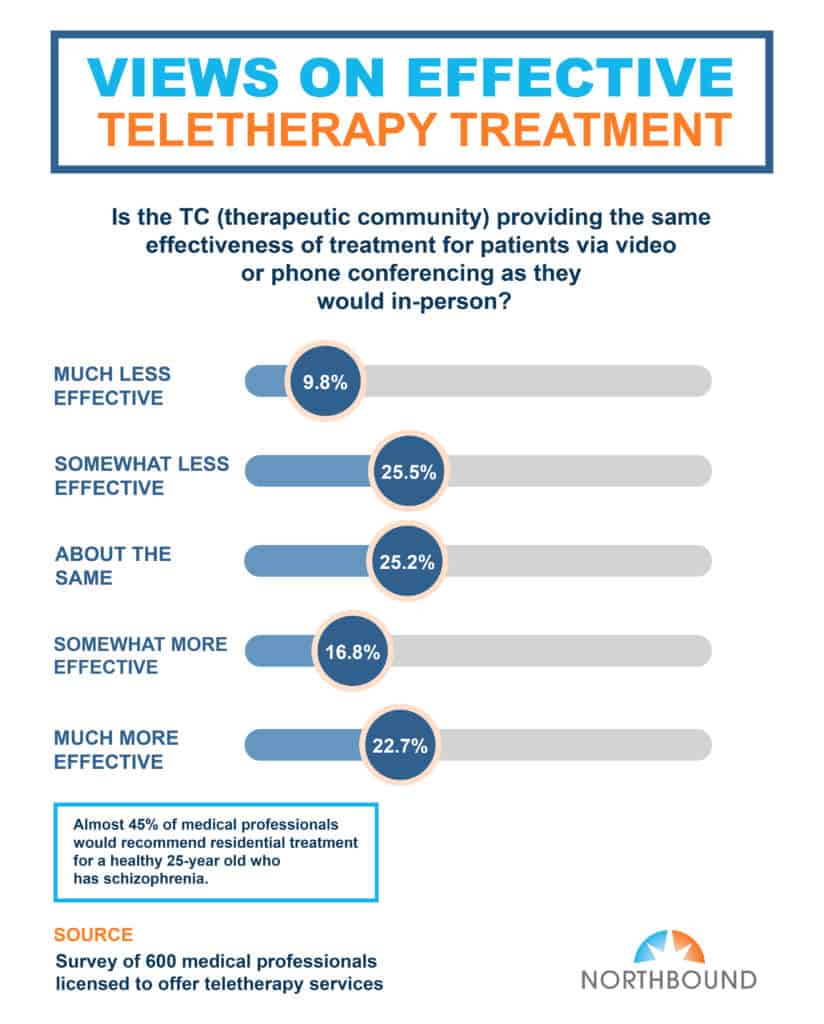
Our survey findings indicate that less than one-fifth (20%) of our participants believe that teletherapy treatment is “somewhat more effective” than in-person counseling. When asked how their mental health has fared throughout COVID-19, one-fourth (25%) rated themselves on the scale as “somewhat worse.”
Psychiatrists and psychiatric social workers agreed that utilizing telehealth services such as video or phone conferencing were slightly more effective than in-person sessions.
One Surprising Benefit to Teletherapy: Patients Aren’t Feeling As Guarded
We found it surprising that while teletherapy does have various benefits (convenience, cost-effectiveness, increased workflow and efficiency, improving patient engagement, quality of healthcare, and patient satisfaction), individuals seemed to not feel as guarded or reluctant to receive help.
Our findings proved that attending therapy sessions virtually from the comfort of your own home can make it easier and more comfortable to receive help for addiction and mental illness as opposed to in-person visits. As mentioned above, telehealth sessions seem to empower more individuals to receive help for their conditions, and most importantly, reduce the stigma that commonly surrounds mental health and addiction treatment. This includes feelings of discrimination guilt, shame, and fear that often arise when going to a rehab facility.
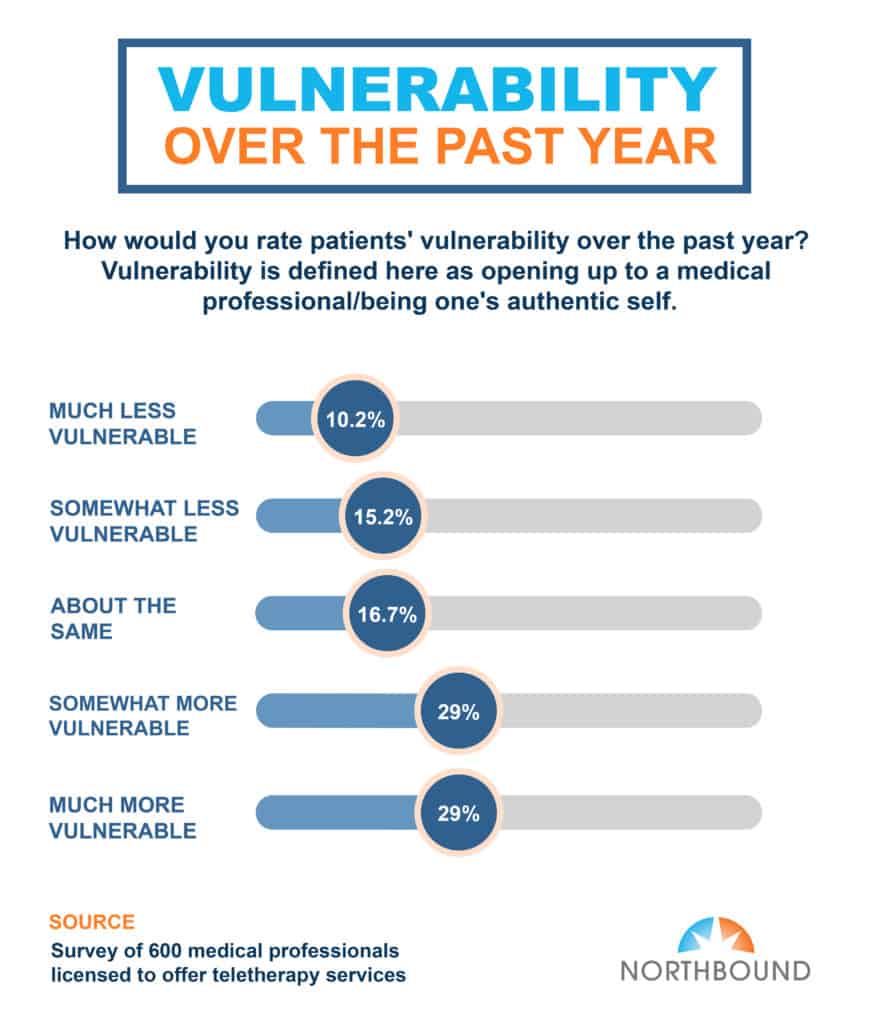
When asked, “How would you rate patients’ vulnerability over the past year?” nearly 3 in 10 (30%) said their clients have been “somewhat more vulnerable.” Vulnerability being defined as opening up/being one’s authentic self.
Medical Professionals Have Mixed Feelings About Long-Term Teletherapy Plans
Millions of Americans experiencing heightened struggles with their mental health during an incredibly tumultuous year found hope and support through teletherapy. This alternative to traditional and in-person patient visits has become a critical resource, not only for those suffering from mental illnesses and addiction, but also to help to reduce the barriers that have stopped people from receiving the mental health treatment they need.
Teletherapy is helping Americans get through COVID-19. But, What happens afterward?
Although medical providers have been in support of the benefits of teletherapy, there is a major question that needs to be asked. What will virtual services look like post-COVID? What we do know from our research, is that medical professionals seem to have mixed feelings about long-term teletherapy plans, because of the previous challenges they have faced.
In-Person Therapy Sessions Are Still Preferred Long-Term Over Teletherapy
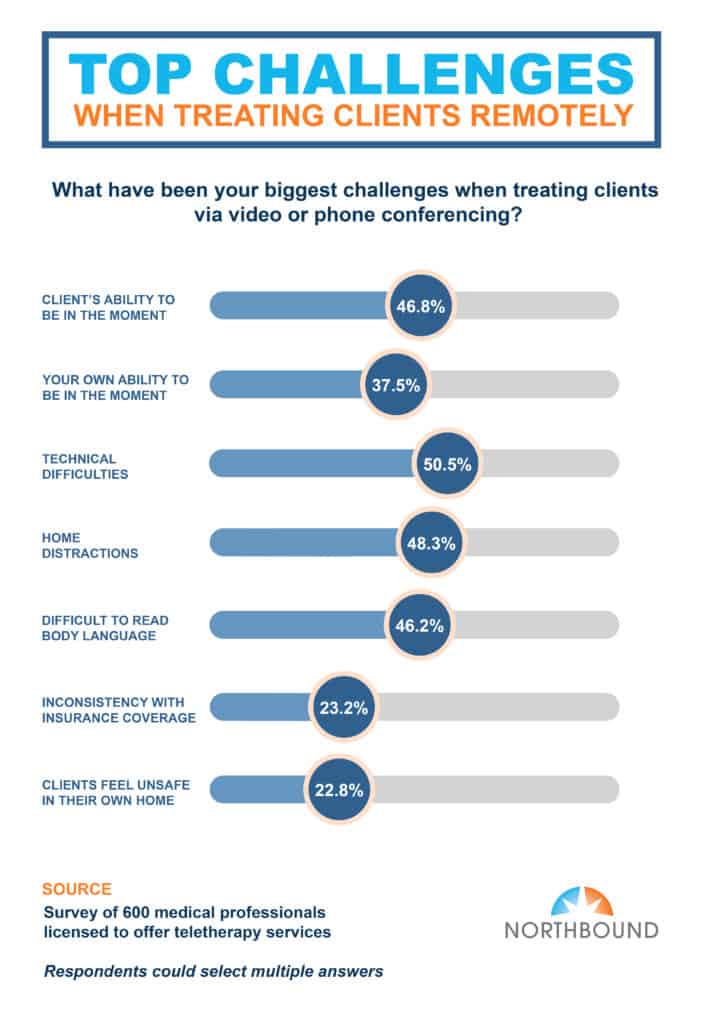
Overall, the respondents of our survey seemed to have positive responses about teletherapy. However, they did note some challenges and issues. These findings indicated the main hurdles medical professionals experience when treating patients virtually, are technical difficulties (50%), home distractions (48%), and a client’s ability to be in the moment (47%).
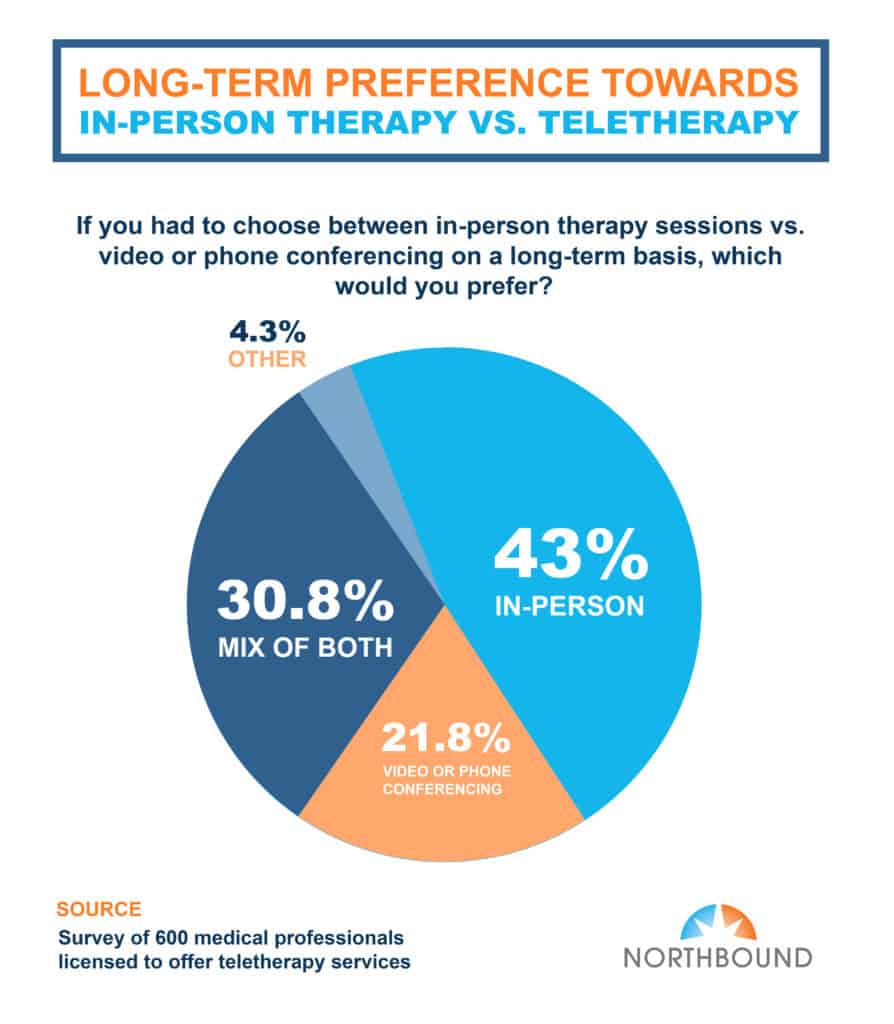
The results also highlighted how patients generally have an easier time opening up during virtual sessions. In fact, less than 17% believe teletherapy treatment is “somewhat more effective” vs. in-person counseling, while 23% of respondents consider remote treatment to be more effective than in-person counseling. However, even with teletherapy being used extensively, results showed that face-to-face therapy is still favored long-term over virtual sessions.
Sources
- https://www.healthcareitnews.com/news/telehealth-use-rises-new-trends-highlight-demographic-divides
- https://www.health.harvard.edu/staying-healthy/telehealth-the-advantages-and-disadvantages
- https://hitconsultant.net/2020/12/30/mental-health-teletherapy-predictions-trends-2021/#.YEZ6yV1Kg-Q
- https://www.vox.com/science-and-health/21427156/what-is-teletherapy-mental-health-online-pandemic
- https://www.nature.com/articles/d41586-021-00175-z
- https://www.healthrecoverysolutions.com/blog/telehealth-and-remote-prescribing
- https://www.washingtonpost.com/lifestyle/wellness/telehealth-teletherapy-mental-health-covid/2020/11/12/fdda8776-242c-11eb-952e-0c475972cfc0_story.html
- https://www.ortholive.com/blog/top-10-benefits-of-telehealth-for-patients-and-doctors/
- https://thelightprogram.pyramidhealthcarepa.com/online-therapy-vs-in-person-therapy/
Methodology
Northbound Treatment Services surveyed a sample of 600 medical professionals using Pollfish. For the analysis, we screened all respondents, ensuring that they are licensed to offer teletherapy services. 285 of which were psychologists, 150 were psychiatrists, and 165 were psychiatric social workers.