Aetna is one of the leading insurance providers in the country, helping millions of people access healthcare that they otherwise would not be able to afford. When it comes to going to rehab for substance abuse, however, Aetna rehab coverage can be tricky. In many cases, Aetna rehab coverage is slim, as is with other insurance companies. However, there are often a few tricks to the trade when it comes to utilizing Aetna rehab coverage when attending a substance abuse program.
How to Determine Aetna Rehab Coverage
Aetna abides by a strict set of protocols that help them determine just how much (if any) Aetna rehab coverage they can provide to an individual looking to receive treatment for substance abuse. Some of the guidelines used to determine if Aetna rehab coverage is possible for individuals in rehab include:
• Milliman Care Guidelines for medical and surgical care
• Aetna Clinical Policy Bulletins
• Centers for Medicare & Medicaid Services (CMS)
• Aetna Level of Care Assessment Tool (LOCAT) for behavioral healthcare
• American Society of Addiction Medicine Patient Placement Criteria for the Treatment of Substance Related Disorders
Those working at Aetna will be able to determine an individual’s Aetna rehab coverage by referring to these protocols and reading between the lines to see if they can provide Aetna rehab coverage.
How Treatment Can Help Obtain Aetna Rehab Coverage
Individuals who are entering into a substance abuse treatment program can also utilize members of the staff who can help maximize the amount of Aetna rehab coverage they can receive. This can include the following:
• Reviewing plans – Most treatment centers will start determining how much an individual’s Aetna rehab coverage will financially help them by reviewing the policy. They will also work to educate the individual on how the policy works, so he or she understands better.
• Working with Aetna – Treatment centers will also make calls to Aetna rehab coverage employees who can help uncover hidden coverage. This can help reduce costs for individuals.
• Plan repayment – If a substance abuse treatment facility is unable to help pinch pennies through using Aetna rehab coverage, then they can help individual’s devise a plan of payment, as well as help provide them with the financial information needed to move forward with their care.
Treatment facilities are often limited to how much they can help implement Aetna rehab coverage, primarily because rehab is generally not covered by Aetna. While in some cases, there might be exceptions to just what kinds of services can be covered through Aetna rehab coverage, in most cases, this coverage often falls short. If you or a loved one are planning on attending a substance abuse treatment program, it is important that you learn about your insurance policy, how much Aetna rehab coverage you might be able to receive, and plan on working with the staff at your facility to determine what your overall costs for care will be. By doing this, you can be prepared for the financial responsibility of care, as well as become educated about Aetna rehab coverage.
Author
-

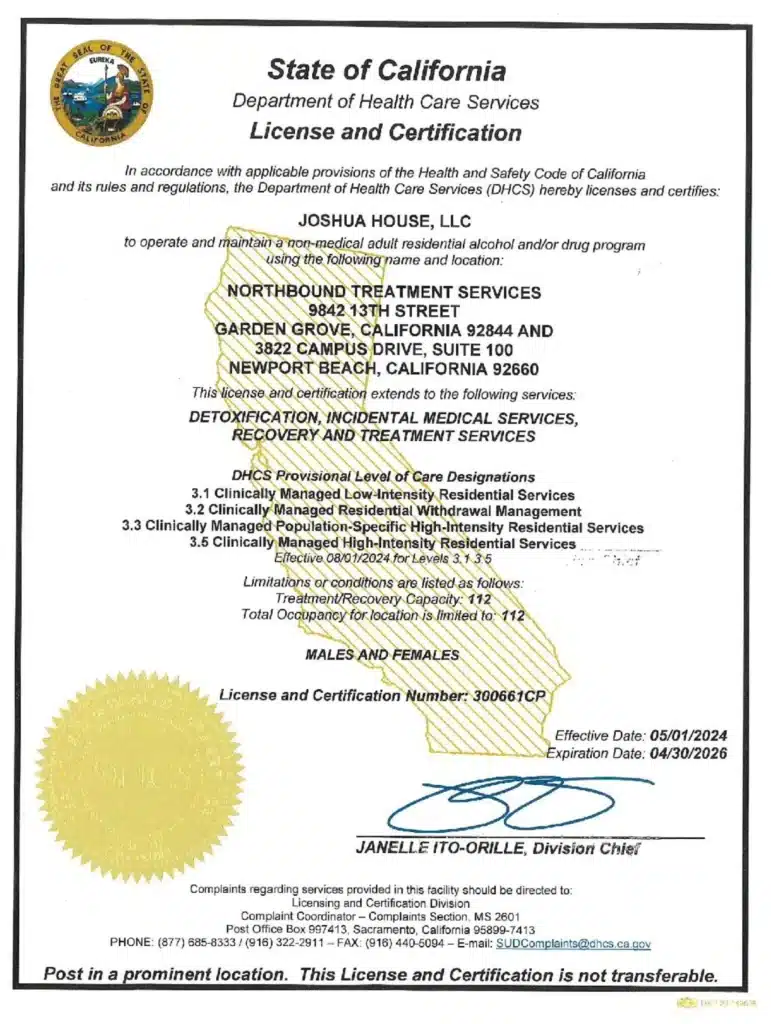
President, CEO & Founder at Northbound Treatment Network
Paul Alexander is the CEO, President & Founder of Northbound Treatment Network in Newport Beach, California. He believes wholeheartedly in transformational leadership, organizational health and effective, fully integrated substance use disorder and mental health treatment. With over 27 years of experience in behavioral healthcare, Paul has extensive knowledge of “in vivo” treatment modalities, clinical development, operations, strategy, marketing and financial planning. He has been widely recognized for his development of collegiate-based residential treatment programs for students in recovery and authored a research study at The University of California confirming this modality’s effectiveness.
Paul’s comprehensive professional experience, willingness to innovate, and emphasis on organizational health are vital factors in Northbound’s continued success. Paul received his Certified Addiction Treatment Specialist training at Saddleback College in Mission Viejo, CA, and was awarded Outstanding Alumni Service Award in 2002. Paul holds a Bachelor of Arts degree in Criminology, Law and Society, Summa Cum Laude, from University of California, Irvine, and a Juris Doctorate degree from Loyola Law School of Los Angeles. Paul currently serves on The National Association of Addiction Treatment Providers (NAATP) board. In addition, he serves on The Family Recovery Foundation board and The CarePossible board in Orange County; both organizations are committed to raising funds for family recovery and treatment for former military personnel. Paul is in recovery himself and lives in Orange County with his wife Silvana and his two young sons, Noah and Dean.