Xanax is a largely familiar brand-name drug known to alleviate anxiety, but is Xanax a benzodiazepine? The answer is yes. The generic name for Xanax is alprazolam and it is part of a family of medications that act as depressants to the central nervous system. In addition to Xanax, other commonly prescribed benzodiazepine drugs are diazepam (Valium) and lorazepam (Ativan).
Benzos work by increasing gamma-aminobutyric acid (GABA) in the brain that helps a person feel relaxed and in a sedative state. It’s often prescribed for anxiety-related disorders as well as insomnia. Due to this group of drugs being highly addictive, they are prescribed for short-term use as a relief and are also used to treat stress, manic behavior, anxiety disorders, and other associated symptoms.
Unfortunately, when it’s not taken correctly or under the care of a medical professional, it becomes easier to create a dependency on the drug. Xanax and other benzos are not meant to use recreationally as a way to self-medicate or achieve any type of “high.” Since Xanax is known as a prescription medication, the risk of addiction may not be as regularly discussed as illicit substances. However, Xanax is quick to take effect and slow to leave the body, easily lending itself to addictive behavior.
Once you become dependent or addicted to Xanax, it’s crucial to seek help from a treatment facility that can help you through the withdrawal period and provide additional therapeutic assistance. Even when properly prescribed, there’s a “weaning off” period of taking Xanax and other benzos to allow the body to adjust without experiencing harmful side effects. Undergoing care at a medically-managed addiction treatment facility can make the process more comfortable, secure, and successful.
Who Is Affected by Xanax Addiction?
It’s reported that Xanax is the number one most prescribed psychiatric medicine in the U.S., meaning it can affect nearly anyone at any time. When taken as prescribed, it deemed mainly safe and effective. Nevertheless, the risk of benzodiazepine addiction still stands when people abuse Xanax or extend their use beyond the set window of time (typically no more than two weeks). When learning how addictive certain drugs are, Xanax is considered one of the main benzos that are associated with dangerous health behavior.
The risk is increased when taking Xanax with alcohol or opioids. This also increases the chance of accidental overdose and experiencing severe side effects. According to the National Institute on Drug Abuse, over 30 percent of overdoses that involve opioids involve benzos. Of all the dangerous drugs there are, Xanax, benzos, and other similar prescriptions didn’t cause as much concern as opioids, but for many, they’re considered just as dangerous.
The Centers for Disease Control and Prevention issued new guidelines in 2016 that recommended doctors to avoid prescribing benzos with opioids due to their adverse effects. Both types of prescriptions now come with a “black box” warning issued by the U.S. Food and Drug Administration that speaks to the dangers of the two combined.
Every person responds to the drug differently both in terms of anxiety relief and negative side effects. Height, weight, age, metabolism, and mental state of mind will affect how quickly your body breaks down and reacts to taking Xanax.
The increase of Xanax use has been a concern for many practitioners, especially among adolescents. In an article published by Pew Research, there have been reports of increased use, with more kids admitted to hospitals for benzo withdrawal symptoms, specifically seizures. Furthermore, a professor at Johns Hopkins University School of Medicine indicates that benzos are “overtaking opioids as the primary prescription drug of abuse in adolescent patients.”
A few of the reasons for the increase of use at a younger age is the increasing number of teens and young adults experiencing anxiety disorders, the availability of Xanax and other benzos, and the misconception about its potential harm when compared to opioids, which are often thought of illicit drugs. As the increase of use rises in individuals, it creates a habit of taking higher doses since benzos eventually stop working.
According to information available through Kaiser Permanente, continuing use of Xanax beyond a two-week window of time results in:
- Loss of effectiveness
- Persistent side effects
- Potential for withdrawal symptoms
- Development of tolerance to the drug and/or dependence
Taking higher doses of Xanax at a greater frequency leads to a buildup in the system, causing the body to become immune to the initial effects of relief. The continuous use of Xanax to meet these same feelings is what leads to substance abuse and eventually addiction.
How Does Xanax Make You Feel?
Xanax affects the central nervous system to help the body feel sedated and relaxed. It’s absorbed quickly into the bloodstream, which allows most people to feel its effects within 15-30 minutes, but these don’t last long. The half-life of Xanax is considerably longer. The half-life refers to how long it takes for a drug to be fully cleared from your system. This can be up to 16 hours, depending on the dosage and a person’s metabolism rate.
The more frequently a person takes Xanax, the faster the body begins to build up a tolerance to the drug, which quickly leads to addiction and subsequent withdrawal symptoms as soon as a person stops taking it. As calming as its effects can be, there are side effects that can be extremely harmful and possibly lead to a medical emergency. Among these are:
- Daytime fatigue
- Muscle weakness
- Loss of balance and coordination
- Confusion
- Lightheadedness
These symptoms are particularly dangerous when operating a motor vehicle or when in a space where you’re unable to lie down or sturdy yourself. These are exacerbated when the use of Xanax is abused and can also be experienced in a cycle with symptoms of Xanax withdrawal, such as:
- Depression
- Hostility or aggressive behavior
- Tremors
- Hallucinations
- Seizures
The pain and discomfort of benzodiazepine withdrawal symptoms are what causes a person to continue using Xanax, but too much, too frequently can result in overdose. The span of time between first taking Xanax and addiction can move quite quickly because of its addicting properties. Once the body becomes used to functioning with this type of benzo in the system, it takes medical care and supervision to safely detox and seek treatment to permanently discontinue use.
What Can I Expect from the Addiction Withdrawal Process?
It’s highly recommended to go through the benzodiazepine dependence withdrawal process under guided supervision and medical support. The physical reactions can be unpredictable to a point that being alone is dangerous. For example, if you experience a seizure or serious tremors, you don’t have full control over your body. Not only does it limit you from being able to receive emergency help, if needed, it can lead to head injuries from falling or other harmful situations, in addition to the side effects you’re already experiencing.
Drug addiction means the body has become used to having Xanax in the system and when it’s no longer present, it can wreak havoc on the body and the mind. Simply not taking the drug isn’t a viable option because addiction deals with the physiological changes to the brain that takes away a person’s ability to “choose” whether to continue taking it or not. Going through detox takes medical monitoring for safety and emotional support to push through the benzodiazepine withdrawal period, as this is taxing and overwhelming to experience.
Withdrawal from Xanax takes up to two weeks and could be longer depending on a person’s history with use. It takes ridding the system of the drug and giving the body time to recalibrate to its new sense of normalcy without the presence of benzos or any other substances. This starts with the detox stage, but is continued with intensive treatment for recovery. Regardless of if a person has become addicted to their prescription or has decided to take Xanax recreationally to “feel good,” there are underlying causes that must be addressed to prevent repeat behavior and to provide healthier solutions.
Seeking Treatment for Xanax Addiction
Xanax abuse can quickly spiral out of control and become addiction. When this happens, treatment is key to safely detox and provide the kind of care needed to treat the initial conditions. People who are prescribed Xanax and end up overmedicating and becoming dependent on the drug still require alternative options to maintain a sense of calm on a regular basis. The same goes for those who struggle with insomnia. When the solution of medication is taken away, there has to be solutions made available through the teaching of safe tools and techniques.
Even if a person’s initial intention was to abuse Xanax, the goal of reaching a certain relaxed state still played a part that lead to physical dependence. As part of treatment, a dedicated team creates a customized plan that identifies certain triggers and behaviors that are likely to lead a person down the same path again and provide ways to handle them in the future. This is done through a combination of individual therapy, group counseling, as well as other activities and education that focus on how to reenter the world without using drugs.
Part of the learning involves going beyond the question of is Xanax a benzodiazepine and identifies a person’s perceived need for use. By getting to the root of the issue versus taking addiction at face value, it helps to prevent the chance of relapse and the introduction of new ways to treat and overcome lingering problems.
Sources:
- Watt, Anthony. “Benzodiazepines: Uses, Side Effects, and Types.” Healthline, Healthline Media, 11 Jan. 2049, www.healthline.com/health/bipolar-disorder/benzodiazepines#1.
- National Institute on Drug Abuse. “Benzodiazepines and Opioids.” 16 Mar. 2018, www.drugabuse.gov/drugs-abuse/opioids/benzodiazepines-opioids.
- Nichols , Hannah. “Xanax: Warnings, Uses, and Side Effects.” Medical News Today, MediLexicon International, 7 Dec. 2017, www.medicalnewstoday.com/articles/263490.php.
- Vestal, Christine. “Teen Xanax Abuse Is Surging.” The Pew Charitable Trusts, 24 Aug. 18AD,
- Holland, Kimberly. “What Does Xanax Feel Like? And 10 Other FAQs About Effects, Dose.” Healthline, Healthline Media, 7 Oct. 2010,
Author
-

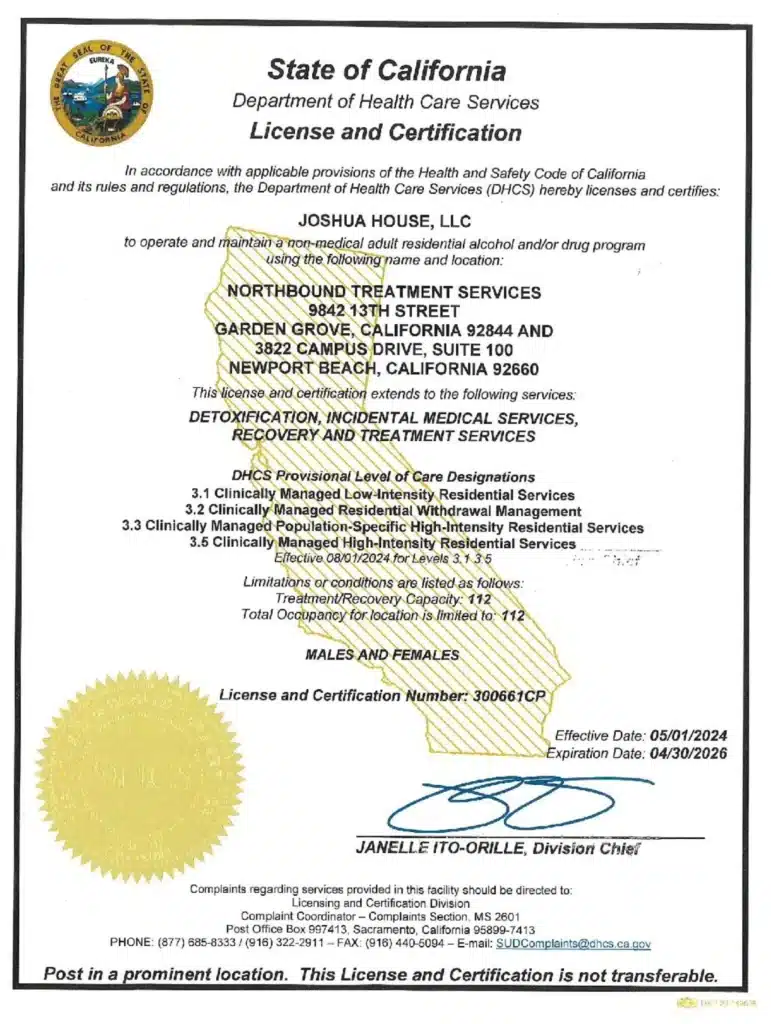
President, CEO & Founder at Northbound Treatment Network
Paul Alexander is the CEO, President & Founder of Northbound Treatment Network in Newport Beach, California. He believes wholeheartedly in transformational leadership, organizational health and effective, fully integrated substance use disorder and mental health treatment. With over 27 years of experience in behavioral healthcare, Paul has extensive knowledge of “in vivo” treatment modalities, clinical development, operations, strategy, marketing and financial planning. He has been widely recognized for his development of collegiate-based residential treatment programs for students in recovery and authored a research study at The University of California confirming this modality’s effectiveness.
Paul’s comprehensive professional experience, willingness to innovate, and emphasis on organizational health are vital factors in Northbound’s continued success. Paul received his Certified Addiction Treatment Specialist training at Saddleback College in Mission Viejo, CA, and was awarded Outstanding Alumni Service Award in 2002. Paul holds a Bachelor of Arts degree in Criminology, Law and Society, Summa Cum Laude, from University of California, Irvine, and a Juris Doctorate degree from Loyola Law School of Los Angeles. Paul currently serves on The National Association of Addiction Treatment Providers (NAATP) board. In addition, he serves on The Family Recovery Foundation board and The CarePossible board in Orange County; both organizations are committed to raising funds for family recovery and treatment for former military personnel. Paul is in recovery himself and lives in Orange County with his wife Silvana and his two young sons, Noah and Dean.