There’s so many health risks associated with substance use disorder that sometimes it seems as if the starkest — death — is camouflaged. But enormous reminders about the reality of that threat continue to surface, no matter how much they’ve been minimized previously.
Three more have come within the last two months alone from the releases of results of extensive, well-funded studies related to drug overdose deaths:
- In its annual mortality report, the National Center for Health Statistics indicates that overdose deaths among young people have fueled the decline in the average life span of Americans for the second straight year.
- Through access to government data on population research, the Centers for Disease Control and Prevention (CDC) were able to determine that the age-adjusted rate of overdose deaths in 2016 was 21 percent higher than in 2015.
- A study of more than 13,000 overdose deaths by researchers at Columbia University Medical Center established that depression and anxiety were the two leading causes of opioid overdose behind chronic physical pain.
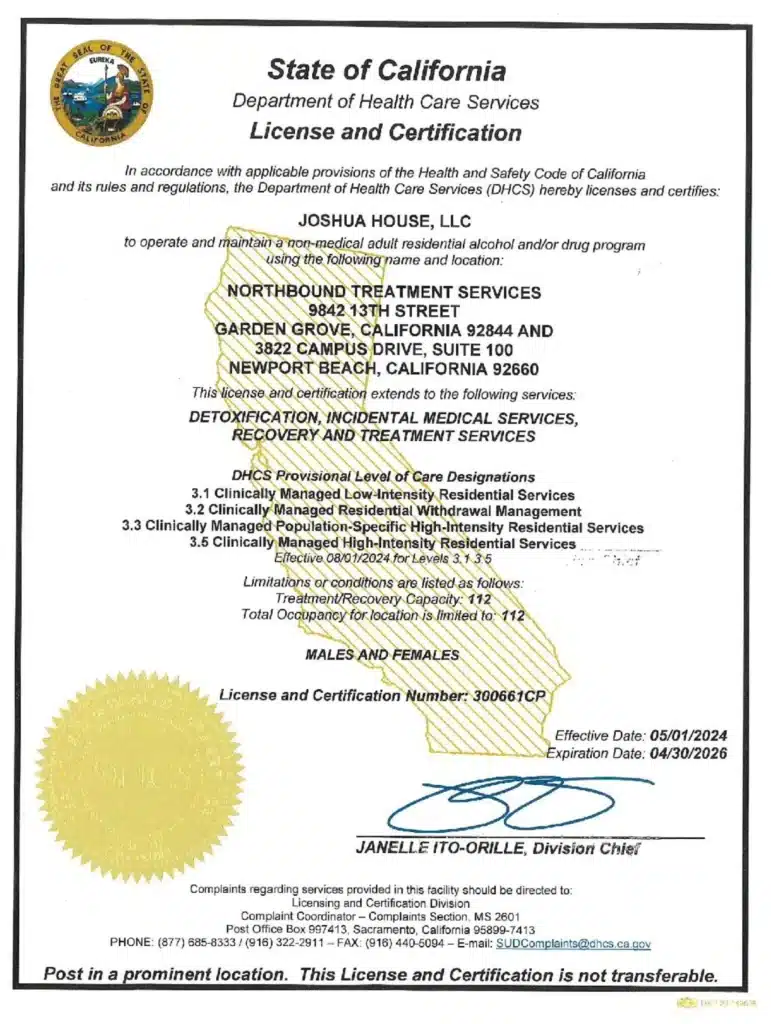
This burst in findings is certainly wearying, further expressing to the grade of treatment centers in the U.S. like Northbound able to clinically assess and manage co-occurring psychiatric and substance use disorders that our work is as pivotal as it’s ever been.
Contributors for “Treatment Retention at Northbound: The Client Advocacy Approach” included Northbound Clinical Director Elizabeth Steele and Client Advocacy Manager Jimmy Weiss.
“The frequent occurrence of treated chronic pain and mental health conditions among overdose decedents underscores the importance of offering substance use treatment services in clinics that treat patients with chronic pain and mental health problems,” stated Dr. Mark Olfson, professor of psychiatry at Columbia University Medical Center and and its lead investigator for the study on overdose deaths.
According to their research, fewer than one out of every 20 of the overdose deaths analyzed came within a short period from when a diagnosis for opioid use disorder was given. Yet approximately one-third of those who died did in fact have a general drug use disorder diagnosed in the year prior.
“Because clinical diagnoses generally indicate treatment, this service pattern suggests that dropout from drug treatment is common before fatal opioid overdose,” Dr. Olfson stated in the report. “Improving treatment retention with contingency management or other effective behavioral interventions might help lower the risk of fatal overdose in these patients.”
Client Advocacy as Treatment Retention
Embedded in Northbound’s strategy for treatment of substance abuse and mental health disorders is the retention objective referred to as Client Advocacy, our extensive approach to equipping each patient with recovery-related resources outside of their therapy that address crisis intervention and early discharge prior to completion. The Client Advocate role is a position on the clinical staff, similar in some ways to the “Recovery Advocate” function commonly applied in the behavioral healthcare structure, but with an explicit shift in focus away from counseling.
Although Client Advocates here are trained to be multi-faceted so they can participate in the process for admissions, treatment extensions, business development and aftercare support, the primary qualifications for the position always remain centered upon their ability to build a meaningful connection with each client.
Client Advocacy was conceptualized to bring that compassion to an extent of protection.
A client’s course to completion of each level of care at Northbound is established through the recommendation of our clinical staff. Yet the therapist oftentimes won’t be integrated with the client in an informal setting, nor will a physician or case manager or even their sponsor. That would contradict the transitional In Vivo (“In Life”) treatment model our clients thrive under due to its engagement with real life experiences.
So a more common human interaction is presented in the form of the Client Advocate, whose protection of clients comes through facilitating their best treatment interests within a basis of trust, particularly if a client gets the urge to, for example, relapse or reach out to an ex-lover against an explicit clinical recommendation not to. Instances like this that have emerged during Northbound’s almost 30 years of treatment service have indicated to us that the disease of addiction is not only very strong, but cunning and baffling as well. At times, clients have offered rationale that makes it easy to understand why they believe it’s beneficial for them to leave treatment.
Our Client Advocates understand those client urges will strike quickly, and that it’s when their protection through advocacy is most critical. In the midst of clients experiencing such triggers, creating space between that impulse and them acting on it has delivered a steady rate of effective outcomes. The position of Client Advocate is truly special.
And the impact of treatment retention is crystal clear. New research is supporting a substantial correlation between overdose deaths and early discharge from care in this era of rampant opioid abuse. That doesn’t account for the many cases out there when more typical effects of untreated co-occurring disorders like behavorial problems (oftentimes leading to incarceration), brain damage symptoms, a severely weakened immune system, etc., were the result. Northbound’s regard for treatment retention with contingency management is apparent in the Client Advocacy approach and the security it offers our clients.
Author
-

President, CEO & Founder at Northbound Treatment Network
Paul Alexander is the CEO, President & Founder of Northbound Treatment Network in Newport Beach, California. He believes wholeheartedly in transformational leadership, organizational health and effective, fully integrated substance use disorder and mental health treatment. With over 27 years of experience in behavioral healthcare, Paul has extensive knowledge of “in vivo” treatment modalities, clinical development, operations, strategy, marketing and financial planning. He has been widely recognized for his development of collegiate-based residential treatment programs for students in recovery and authored a research study at The University of California confirming this modality’s effectiveness.
Paul’s comprehensive professional experience, willingness to innovate, and emphasis on organizational health are vital factors in Northbound’s continued success. Paul received his Certified Addiction Treatment Specialist training at Saddleback College in Mission Viejo, CA, and was awarded Outstanding Alumni Service Award in 2002. Paul holds a Bachelor of Arts degree in Criminology, Law and Society, Summa Cum Laude, from University of California, Irvine, and a Juris Doctorate degree from Loyola Law School of Los Angeles. Paul currently serves on The National Association of Addiction Treatment Providers (NAATP) board. In addition, he serves on The Family Recovery Foundation board and The CarePossible board in Orange County; both organizations are committed to raising funds for family recovery and treatment for former military personnel. Paul is in recovery himself and lives in Orange County with his wife Silvana and his two young sons, Noah and Dean.